What is the Lipid Profile? A Comprehensive Guide to Understanding, Analyzing, and Managing Cholesterol Levels
Managing our health often requires understanding specific tests and metrics that can indicate the state of our well-being. One such essential test is the Lipid Profile, sometimes referred to as the Lapid Profile. This blood test provides valuable insights into the levels of cholesterol and fats in your blood, helping to assess the risk of cardiovascular diseases and guide treatment plans. In this article, we will explore what the Lipid Profile is, why it is important, how to analyze its results, factors that can cause abnormalities, and ways to prevent these issues. We will also include insights from top doctors, real-life patient stories, and links to reputable labs specializing in lipid management.

What is the Lipid Profile?
The Lipid Profile is a comprehensive blood test that measures the levels of different types of fats (lipids) in your blood. It typically includes the following components:
Total Cholesterol: This measures the overall amount of cholesterol in your blood, including both low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol.
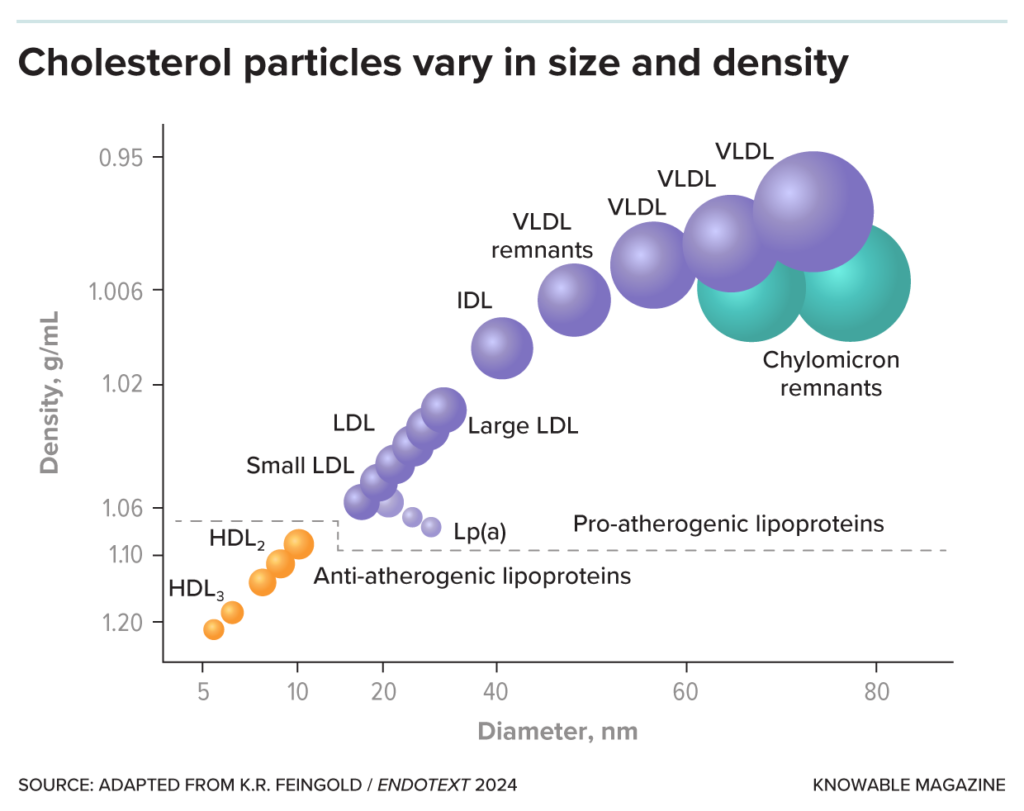
Low-Density Lipoprotein (LDL) Cholesterol: Often termed as “bad cholesterol,” high levels of LDL can lead to plaque buildup in your arteries, increasing the risk of heart disease and stroke.
High-Density Lipoprotein (HDL) Cholesterol: Known as “good cholesterol,” HDL helps remove other forms of cholesterol from your bloodstream, lowering the risk of heart disease.
Triglycerides: A type of fat found in your blood. Elevated triglycerides can increase the risk of cardiovascular diseases, particularly in individuals with diabetes or metabolic syndrome.
Very Low-Density Lipoprotein (VLDL) Cholesterol: This is a type of lipoprotein that carries triglycerides in your blood. High VLDL levels can also contribute to plaque buildup in your arteries.
Visual Summary: Understanding Your Lipid Profile
| Component | Ideal Range | Potential Health Risks of Abnormal Levels |
|---|---|---|
| Total Cholesterol | Less than 200 mg/dL | 200-239 mg/dL (Borderline High): Increased risk of heart disease. 240 mg/dL and above (High): Significantly raises cardiovascular risk. |
| LDL Cholesterol | Less than 100 mg/dL | 100-129 mg/dL (Near Optimal): Monitor closely. 130-159 mg/dL (Borderline High): Increased risk of plaque buildup. 160-189 mg/dL (High): High risk of heart disease. 190 mg/dL and above (Very High): Very high risk of heart attack or stroke. |
| HDL Cholesterol | 60 mg/dL and above | Less than 40 mg/dL (Low): Increased risk of heart disease. High HDL (60 mg/dL and above) is protective against heart disease. |
| Triglycerides | Less than 150 mg/dL | 150-199 mg/dL (Borderline High): Increased cardiovascular risk. 200-499 mg/dL (High): Significant risk of heart disease. 500 mg/dL and above (Very High): Risk of pancreatitis and cardiovascular disease. |
| VLDL Cholesterol | 5-40 mg/dL | Elevated VLDL is associated with higher triglyceride levels and increased risk of heart disease. |
Why is the Lipid Profile Important?
The Lipid Profile is a crucial tool in preventive healthcare because it helps identify people at risk for cardiovascular diseases, including heart attacks and strokes. Here’s why it’s important:
Early Detection of Cardiovascular Risk: Abnormal lipid levels are a major risk factor for heart disease, which is the leading cause of death worldwide. Identifying and managing these levels early can significantly reduce the risk of serious complications.
Guiding Treatment Plans: Depending on your Lipid Profile results, your doctor can recommend lifestyle changes, medications, or further tests to manage your cardiovascular risk. This personalized approach can prevent the progression of heart disease.
Monitoring Chronic Conditions: For individuals with conditions like diabetes, high blood pressure, or metabolic syndrome, regular Lipid Profile tests are essential to monitor the effectiveness of treatment and make necessary adjustments.
Analyzing the Lipid Profile: What Do the Numbers Mean?
Understanding your Lipid Profile results is key to managing your health. Here’s a breakdown of what the numbers mean:
- Total Cholesterol:
- Desirable: Less than 200 mg/dL
- Borderline High: 200-239 mg/dL
- High: 240 mg/dL and above
- LDL Cholesterol:
- Optimal: Less than 100 mg/dL
- Near Optimal: 100-129 mg/dL
- Borderline High: 130-159 mg/dL
- High: 160-189 mg/dL
- Very High: 190 mg/dL and above
- HDL Cholesterol:
- Low (increased risk): Less than 40 mg/dL for men and less than 50 mg/dL for women
- Desirable: 60 mg/dL and above
- Triglycerides:
- Normal: Less than 150 mg/dL
- Borderline High: 150-199 mg/dL
- High: 200-499 mg/dL
- Very High: 500 mg/dL and above
- VLDL Cholesterol:
- Normal: 5-40 mg/dL
The Role of LDL Particle Size in Cardiovascular Risk
Not all LDL cholesterol is created equal. Recent research has shown that the size of LDL particles plays a significant role in cardiovascular risk. Smaller, denser LDL particles are more likely to penetrate the arterial walls and cause plaque buildup, leading to a higher risk of heart disease compared to larger, less dense particles. This aspect of lipidology is becoming increasingly important in advanced lipid testing and risk assessment.
Real-Life Story: Managing High Cholesterol with Lifestyle Changes
Meet John, a 52-year-old man with a family history of heart disease. Last year, John’s Lipid Profile showed alarmingly high LDL levels (180 mg/dL) and triglycerides (300 mg/dL). His doctor, Dr. Lisa Kallin from the Cleveland Clinic, advised immediate lifestyle changes, including adopting a Mediterranean diet, increasing physical activity, and quitting smoking. Over the next six months, John transformed his lifestyle, losing 20 pounds, and his Lipid Profile improved dramatically: his LDL dropped to 110 mg/dL, and triglycerides to 140 mg/dL.
“I always knew I had to take care of my health, but seeing the numbers on my Lipid Profile really made it real for me,” John says. “It was a wake-up call. I’m so grateful to Dr. Kallin for helping me turn my health around.”
When is a Lipid Profile Test Recommended?
Doctors recommend a Lipid Profile test for:
- Routine Health Check-Ups: Starting at age 20, adults should have their Lipid Profile checked every 4-6 years. More frequent testing may be required for those with a family history of heart disease or other risk factors.
- Diabetes or Hypertension Management: People with diabetes or high blood pressure should have regular Lipid Profile tests to monitor cardiovascular risk.
- Existing Heart Conditions: Patients with a history of heart disease or stroke need frequent lipid monitoring to prevent further complications.
Factors That Can Cause Elevated Lipid Levels
Elevated lipid levels can result from a variety of factors, including:
Dietary Habits: Diets high in saturated fats, trans fats, and cholesterol can raise LDL and total cholesterol levels. Foods such as red meat, full-fat dairy products, and fried foods are common culprits.
Lack of Physical Activity: A sedentary lifestyle can lower HDL (good cholesterol) levels and raise triglycerides, increasing cardiovascular risk.
Obesity: Being overweight or obese is linked to higher levels of LDL and triglycerides and lower levels of HDL.
Genetics: Familial hypercholesterolemia is a genetic condition that leads to very high LDL cholesterol levels and an increased risk of early heart disease.
Smoking: Smoking lowers HDL cholesterol and damages blood vessel walls, making them more susceptible to plaque buildup.
Excessive Alcohol Consumption: Drinking too much alcohol can raise triglyceride levels significantly.
Medical Conditions: Conditions like hypothyroidism, kidney disease, and liver disorders can lead to abnormal lipid levels.
Medications: Certain medications, such as steroids and diuretics, can affect lipid levels.
Ways to Prevent and Manage High Lipid Levels
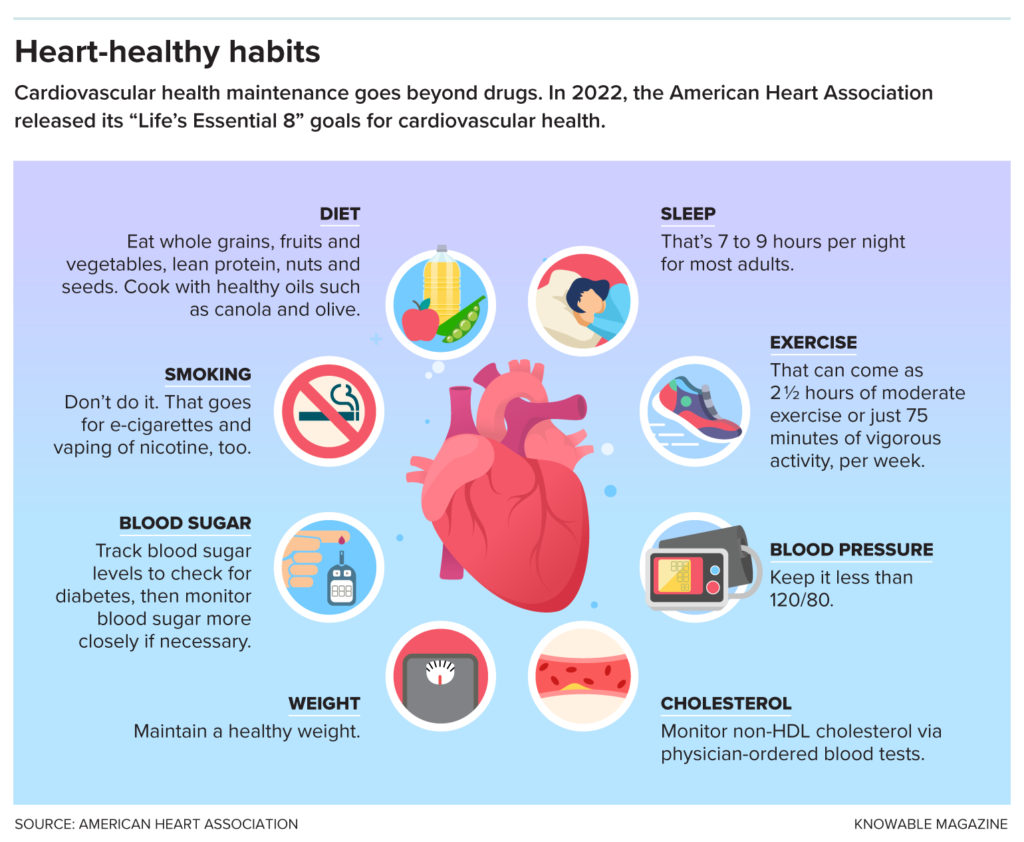
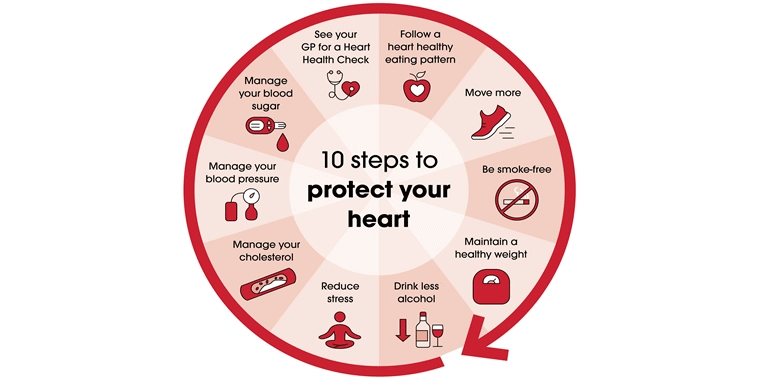
Managing lipid levels effectively requires a combination of lifestyle changes and, in some cases, medication. Here are evidence-based strategies to maintain healthy lipid levels:
Adopt a Heart-Healthy Diet
- Increase Fiber Intake: Foods high in soluble fiber, such as oats, fruits, and vegetables, can help reduce LDL cholesterol.
- Choose Healthy Fats: Replace saturated and trans fats with healthier fats found in olive oil, avocados, and fatty fish like salmon.
- Limit Sugar and Refined Carbs: High sugar intake can raise triglycerides. Opt for whole grains instead of refined grains.
- Include Plant Sterols and Stanols: These naturally occurring substances found in plants help lower cholesterol by blocking its absorption in the intestine.
- Consider Supplements Carefully: Supplements like plant sterols, stanols, and omega-3 fatty acids may help manage cholesterol levels. However, always consult a doctor before starting any supplement regimen.
Exercise Regularly
- Aim for at least 150 minutes of moderate aerobic exercise per week, such as brisk walking, or 75 minutes of vigorous exercise, such as running. Exercise can help lower triglycerides and raise HDL cholesterol.
**Maintain a Healthy Weight**
- Losing even a small amount of weight can help lower cholesterol levels. Focus on a balanced diet and regular physical activity.
Avoid Smoking and Limit Alcohol Consumption
- Quitting smoking can improve your HDL cholesterol level and benefit your heart and blood vessels. Limiting alcohol can prevent triglyceride spikes.
Medications
- For some, lifestyle changes alone may not be enough. Medications like statins, niacin, or fibrates can be prescribed to help manage cholesterol levels.
Alternative Therapies and Supplements
Some people turn to alternative therapies, such as red yeast rice or garlic supplements, to manage their cholesterol levels. While these may have some beneficial effects, it is essential to consult a healthcare provider before using any alternative treatments, as they can interact with medications or have side effects.
Potential Benefits of Supplements:
Supplements for Cholesterol Management
- Plant Sterols and Stanols are natural substances found in plants that can help reduce cholesterol levels. They work by blocking the absorption of cholesterol in the intestines, which can lead to lower LDL (“bad”) cholesterol levels without affecting HDL (“good”) cholesterol. Including foods fortified with plant sterols and stanols, such as certain margarines, orange juice, and yogurt drinks, can be an effective way to help manage cholesterol.
- While these supplements can be beneficial, it’s essential to consult with a healthcare provider before starting any new supplement regimen. A healthcare professional can provide personalized advice based on your health history and current medications, ensuring that you make informed decisions about your cholesterol management.

Top Doctors’ Opinions and Resources
Here’s what leading experts have to say about the importance of the Lipid Profile and managing cholesterol levels:
- Dr. Daniel Rader, Cardiologist at the University of Pennsylvania: “Understanding your lipid levels is crucial in assessing your risk for cardiovascular disease. While lifestyle changes are the cornerstone of management, medication is often necessary for those with genetic predispositions or very high levels.”
- Dr. Elizabeth Klodas, Preventive Cardiologist: “Diet plays a significant role in managing cholesterol. Plant-based diets rich in fiber and healthy fats can dramatically improve lipid levels without medication in many cases.”
- Dr. Dariush Mozaffarian, Cardiologist and Epidemiologist: “Small, dense LDL particles are a major risk factor for heart disease. Advanced lipid testing that measures particle size can provide more detailed insights into cardiovascular risk than standard lipid panels.”
Patient Education Resources:
- American Heart Association: Cholesterol Management
- National Institutes of Health: High Cholesterol
- Cleveland Clinic: Lipid Management Program
Recommended Labs for Lipid Profile Testing
For accurate and comprehensive lipid testing, consider the following reputable labs:
- Quest Diagnostics: Offers extensive lipid panel testing and advanced lipid particle testing.
- LabCorp: Provides a variety of lipid profile tests and advanced cardiovascular testing options.
- Cleveland HeartLab: Specializes in cardiovascular risk testing, including advanced lipid panels and inflammatory markers.
Call to Action: Take Charge of Your Heart Health
If you haven’t had your Lipid Profile tested recently, now is the time to do it. Discuss your results with your healthcare provider to create a personalized plan to manage your lipid levels and reduce your cardiovascular risk. Share this information with friends and family to help them stay informed and proactive about their heart health.
Final Call-Out:
- “Did You Know?”: Heart disease is the leading cause of death globally, but it’s largely preventable with the right lifestyle changes and medical care. Don’t wait—schedule your Lipid Profile test today!
By understanding and managing your lipid levels, you can take a proactive step towards a healthier, longer life. Remember, knowledge is power, and taking control of your health starts with understanding what’s happening inside your body.
for more information







One Comment
Comments are closed.